As a Diabetes Educator, I strive to help each and every one of my patients obtain the best possible control of their blood sugars and live the healthiest lives possible. I mean, that’s my job after all, right? But actually, I happen to know that the most important person to help you manage your diabetes is YOU.
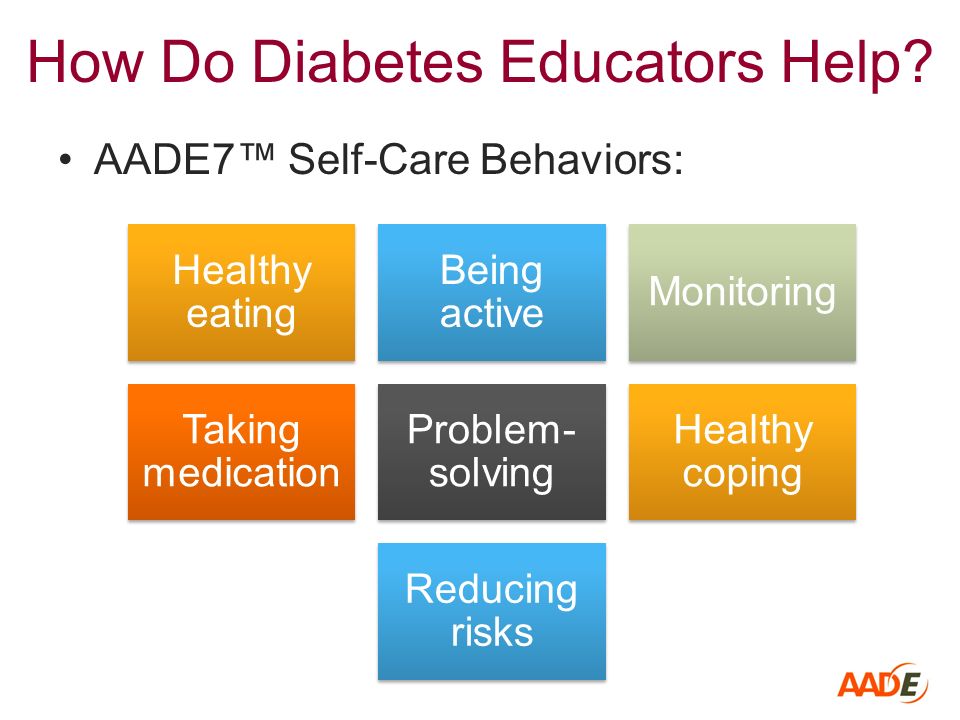
The American Association of Diabetes Educators (AADE) has outlined the seven most important components of diabetes self-care management, known as the AADE7. Diabetes Educators use these as the foundation to help guide their patients through the journey of self-management.
How well are you doing with your self-care?
1. Healthy Eating
What and how much you eat plays a huge role in the control of your blood sugars. Proper timing, modest portions and well-balanced meals are the cornerstones of healthy eating. A well-balanced intake consists of lean proteins, lots of non-starchy vegetables, some low-fat dairy, fruit, whole grains, and a little heart-healthy fat. It’s also important to limit your intake of carbohydrate foods, which have the largest effect on your blood sugars. Carbohydrates include fruit & fruit juice, milk & yogurt, grains, beans, and starchy vegetables. Reading food labels for total carbohydrate is one of the best ways to help you limit your intake. Most adults only need about 45-60 grams of carb at each meal. A diabetes educator can help you put together a healthy meal plan.
2. Being Active
Moving your body every day is so important for our overall health and well-being. It helps to lower your blood sugars, it’s good for your heart, it can help maintain strong bones, it can reduce stress, and it can help you control your weight. You don’t need a fancy gym membership or exercise equipment to be active. Walking is a fantastic, free and easily accessible form of physical activity for most people with diabetes. Many people enjoy using fitness trackers to count their steps. The goal is 10,000 steps a day, or 150 minutes of physical activity a week. That may sound really overwhelming for some people. Start off slow! Even just 10 minutes a day is a great start. Also, focusing on just “sitting less” can help to increase your physical activity level. For those with physical limitations, talk with your doctor or diabetes educator for alternative ways to move. And always talk to your doctor before you begin any exercise program.
3. Monitoring
Testing your blood sugar on a regular basis is the best way to know how well you are managing your diabetes. I like to see my patients test their blood sugar twice a day. One of the best times to test your blood sugar is first thing in the morning, before eating or drinking anything. This is called your fasting blood sugar. The goal for your fasting blood sugar is less than 130. Another great time to test is two hours after you start eating a meal. Testing your blood sugar at this time tells you how well your body is handling the amount of carbohydrate you are eating. The blood sugar goal after a meal is less than 180. If you are consistently seeing blood sugars above 180 after meals, you may be eating too many carbohydrates, or your body may need more medication to help keep your blood sugar in the target range. It’s important to tell your doctor right away if your blood sugars are consistently above these target goals. If you do not have a meter to test your blood sugars, tell your doctor you are interested in self-monitoring your blood glucose. It’s one of the best tools you have to make sure your blood sugars are in the healthiest range.
4. Taking Medication
There are many different medications that are helpful in lowering blood sugar. You may have been prescribed oral medication, insulin, non-insulin injectables, or a combination of these. If your doctor has prescribed medication to help control your blood sugar, it’s important to take it exactly as prescribed in order for it to do its job. If you often miss or forget a dose, try placing your pills next to the coffee maker or on top of your dinner plates. Some people find it helpful to set reminders to go off on their phone.
5. Problem Solving
There are certainly going to be times when your blood sugars go a lot higher or lower than they should. (A low blood sugar is anything lower than 70). You want to be able to help yourself figure out why that may have happened. Think about what may have been different from the usual. If your blood sugar went up too high, did you eat too many carbs? Eat too large of portions? Forgot your meds? How about if your blood sugar goes too low? Did you go too long between meals? Or not eat enough carbohydrates? Take too much insulin? If you can figure out what caused the problem, you can come up with solutions for the next time and learn from that mistake.
6. Reducing Risks
Having diabetes increases your risk of heart attack and stroke, as well as other complications such as kidney disease, retinopathy of your eyes and nerve damage to your legs and feet. It’s important to visit your doctor on a regular basis, at least once a year. If your diabetes is out of control, you should visit more often. It’s also highly recommended that you visit your dentist every six months and your eye doctor once a year. Smoking and diabetes are a bad, bad combination; so if you smoke, talk your doctor about ways to help you quit. Finally, make sure to take good care of your feet. Look for open sores everyday (use a mirror if you need to) and take your socks off at your doctor’s visit and ask your doctor to exam your feet.
7. Healthy Coping
We all know that life is filled with stress. Dealing with diabetes can often add to that stress. Because stress can raise your blood sugars, finding healthy ways to deal with that stress is an important part of your diabetes self-management. There are a lot of ways to help you cope with stress. Some of the best stress relievers include daily physical activity, meditation, or developing a hobby that can take your mind off daily stress. It’s also important to seek the support of your friends and family or even join a diabetes support group.
By concentrating on each and every one of these self-care behaviors, you can feel confident you are taking the best possible care of yourself and your diabetes. Remember, that your doctor and your diabetes educator are always there to help support you in this journey, but the most important person responsible for managing your diabetes is YOU!
By Annie Fanberg, RD, CDE
Cecelia Health Certified Diabetes Educator