As costs continue to rise in the healthcare industry and payer quality measures become increasingly important, effective chronic disease management is more critical than ever. However, without adequate patient engagement and care coordination strategies, efforts to improve health outcomes of those with chronic conditions will not be successful.
For health plan members living with diabetes, positive health outcomes can be particularly hard to come by. Despite education initiatives and care plans in place, even the most committed individuals find it tough to adopt and adhere to a self-care regimen. In addition to the challenges of managing their diabetes, most adults with diabetes have at least one comorbid chronic disease and up to 40% have at least three.
For many payers, diabetes management programs designed to move the needle on Star, HEDIS, and other quality measures have fallen flat as hard-to-reach or underserved members continue to struggle with self-management. This page discusses strategies for improving diabetes health outcomes through more effective member engagement.
The Challenge: Engaging High-Cost Members with Diabetes
Often, diabetes care initiatives, including technology-based apps and payer-sponsored education programs, are designed to reach those who are already inclined to self-manage their conditions. On the other side of the coin, the small population of members who are at-risk, underserved, or do not seek help managing their conditions are driving the majority of diabetes-related costs for payer organizations.
Just 18% of health plan members with diabetes represent 40% of the cost to payer organizations. Various studies show the true scope of the issue.
Various studies show the true scope of the issue.
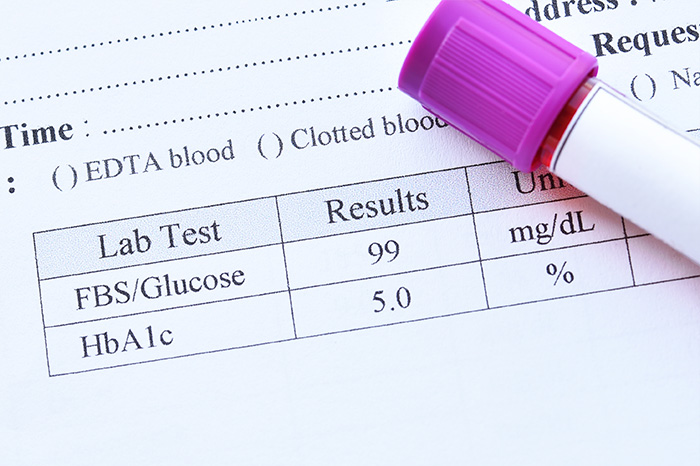
- At least 45% of patients with type 2 diabetes fail to achieve adequate glycemic control (HbA1c <7%) (Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors)
- 50% of medications for chronic diseases are not taken as prescribed (National Institute of Diabetes and Digestive and Kidney Diseases)
- Only 13.2% of people with diabetes achieved target levels for blood pressure, cholesterol levels, and glucose control. (American Diabetes Association)
Value-based care models have been one solution adopted by many payers in recent years to address the lack of positive health outcomes. However, A 2017 study published in Health Affairs suggested that although value-based care programs improved patient access to care, drove care coordination, and reduced emergency department visits, they did not yield the cost savings to cover management costs.
For high-risk and poorly controlled members with diabetes, education alone is often not enough to drive the deep behavioral changes needed to make a positive impact on costs and quality measures. Yet these mindset, lifestyle, and behavior changes are the keys to achieving benefits for the payer, provider, and patient alike.
Benefits of Driving Patient Behavior Change
- Improve patient self-efficacy and health outcomes by increasing the patient’s knowledge, attitude, and behaviors
- Support providers in value-based arrangements and improve quality of care by closing feedback loops and gaps in care
- Increase payer reimbursement potential by meeting or exceeding thresholds for quality and clinical outcomes
The challenge in reaching these opportunities is that each individual faces unique barriers when it comes to adopting and adhering to a diabetes care plan, and overcoming those barriers is extremely difficult for payer programs to achieve at scale.
Barriers to Care Plan Adherence
Reasons for care plan nonadherence are varied and complex. Here are some of the most common barriers to care plan adherence faced by diabetes patients.
Lack of acceptance of the diagnosis
People who are struggling to accept their diabetes are much less likely to initiate and adhere to care plans or educate themselves about their condition. There are many reasons why someone may initially not accept their diabetes diagnosis. Here are some common reasons for a lack of acceptance:
- The person is asymptomatic or rarely experiences symptoms.
- The person is not educated about diabetes.
- They feel a loss of independence and ability to live life on their terms, so they simply decide to live as if they do not have diabetes.
Feeling fearful or overwhelmed
Another common emotion patients experience after receiving a diabetes diagnosis is fear. The fear can take many shapes, including:
- Fear of the unknown—what is going to happen to me?
- Fear of managing their condition
- Fear of administering their medication or checking their blood sugar levels
- Fear of increased doctor visits
- Fear of side effects

Incorrect perceptions of condition or medication
Often, general practitioners who don’t specialize in diabetes don’t have the time or training to properly educate patients on their condition, even in value-based arrangements. This can lead the patient to develop misconceptions about their disease.
Patients may gauge the necessity of treatment based on their perception of their current state, rather than following the recommendations of a health professional.
While fear or denial can play a role in this pattern, a more common challenge is the patient not fully understanding their care plan.
Struggling with financial resources
Diabetes is a disease that disproportionately affects low-income individuals. At the same time, diabetes self-management presents some of the biggest challenges for people who struggle with financial resources.
A low-income status affects nearly every aspect of diabetes self-management. Low-income individuals may not always have reliable access to their medications. Other potential barriers that can affect adherence include food insecurity, lack of access to safe and affordable exercise, and low health literacy.
Literacy or language barrier
High-risk populations of diabetes patients may face barriers of comprehension when it comes to adhering to their care plans. Low health literacy or a language barrier with a care provider can lead to a lack of understanding of the importance of self-management and the steps needed to ensure positive health outcomes.
Challenges with lifestyle changes
When faced with a life-altering diagnosis, it can often be difficult to accept that certain lifestyle changes need to be made to properly manage the condition. Many diabetes patients struggle with changing their diets and exercise habits when first faced with the diagnosis. This challenge also extends to taking their medication.

Access to care
For a variety of different reasons, many people living with diabetes struggle with access to the necessary care to properly manage their conditions. Lack of access to care can include:
- Lack of availability of services
- Prohibitive healthcare and prescription costs
- Lack of patient mobility
- Difficulty getting to the doctor or pharmacy
90% of chronic disease management occurs outside the acute care setting.
Behavior Changes That Generate Measurable Health Improvements
For high-risk and poorly controlled populations, improving health outcomes and quality measures requires a holistic focus on a variety of different areas. To be truly effective and impactful, member engagement programs must focus on all of the following key topics:
Lifestyle change
Changing habits and ingrained behaviors is challenging for anyone, but can be especially daunting for those living with diabetes. Lifestyle changes are often needed in the areas of nutrition and exercise, and can also extend to substance-related habits.
A1C reduction
A 1-point reduction in A1C reduces the rate of heart attack, stroke, or risk of death from cardiovascular causes by 57%. A 1-point reduction also reduces the risk of kidney disease by 50% and eye disease by 76%.
Medication adherence
For people living with diabetes, medication adherence is a critical aspect of managing the condition and living healthier lives. Medication adherence is linked to positive clinical outcomes, while low adherence has proven to lead to increased morbidity and mortality, with a greater risk of a major adverse cardiac event.
Closing gaps in preventive care
Diabetes often leads to related complications, and preventive care is essential to preventing and treating these issues. However, for a variety of reasons, many people experience gaps in diabetes care, which directly contributes to lower HEDIS measures for eye, kidney, and blood pressure exam requirements.

Improving self-management confidence
As previously discussed, many complex barriers can contribute to a lack of confidence in diabetes self-management, from fear to lack of health literacy to lack of understanding of prescription instructions. For patients to successfully improve their health, they need confidence in their care plans and their ability to self-manage their disease.
Success Factors for Achieving Behavior Change
As we have seen, making deep mindset and behavior changes changes is challenging for a wide variety of reasons. Only through the caring experience of human connection can underserved diabetes populations begin to confidently self-manage their conditions.
At Cecelia Health, we have successfully worked with health plans of all sizes to improve the health of their members with diabetes with direct, measurable impacts on Star, HEDIS, and Healthy Days measures. Our approach complements and integrates with existing client programs and resources and builds upon the successes and lessons learned with payer, provider, pharma, and device clients.
We combine the individualized coaching of an expert clinician and proprietary technology to deliver a personalized coaching program to improve self-management and drive behavior change. Cecelia Health focuses on high-risk, poorly controlled populations who face unique barriers or would otherwise not seek help.

With the care and attention of a CDCES, we can strengthen the education for all patients, and meet them where they are to make significant positive changes.
Here are the success factors our approach uses to achieve measurable improvements in health outcomes.
Certified Diabetes Care and Education Specialists
Certified Diabetes Care and Education Specialists (CDCESs) are health professionals who work one-on-one with patients to help identify their personal barriers and teach strategies for overcoming them. CDCESs educate, support, and advocate for people affected by diabetes, as well as promote self management to achieve individualized behavior and treatment goals.
CDCESs can help people living with diabetes in many ways. Successful self-management involves a broad range of topics, and it is the CDCES’s goal to identify the key areas for improvement facing each individual. CDCESs can help individuals focus on:
- Medication
- Nutrition
- Exercise
- Coping skills
At Cecelia Health, our CDCES coaches are experts at building trusted relationships with patients. Each CDCES has a clinical background (RD, RN, PharmD, etc.), is technology-fluent and product-fluent, and culturally competent. Many are also multilingual. We ensure that our team of CDCESs has the right background to reach and engage with high-risk, poorly controlled, and underserved populations.
Scalable personalized coaching
With the personalized approach of a CDCES, people living with diabetes can become empowered to improve their lives and achieve measurably improved health outcomes. Cecelia Health leverages technology and intelligent clinical algorithms to effectively scale the CDCES-patient relationship at a high volume, while driving program quality and consistency.
CDCESs provide patients essential one-on-one support in between provider visits. Through remote communication and monitoring technology, Cecelia Health has identified how to reach hundreds of thousands of patients with the support of a caring CDCES.
Personalization is critical to improving health outcomes for individuals. One reason support from a CDCES is so effective is because CDCESs truly care about their patients as people. They get to know each individual—not just their medical history, but who they are. CDCESs empathize with patients and show genuine understanding for their struggles. By doing so, they build trust, and patients become more likely to follow the CDCESs advice.

Meaningful goals
Cecelia Health’s approach focuses on helping patients set and achieve meaningful goals to improve overall health outcomes. To measure success of the goals, we use the SMART framework; patient goals are Specific, Measurable, Attainable, Relevant, and Timely. Goals address issues in the following areas:
- Nutrition
- Blood glucose monitoring
- Physical activity
- Preventive care
- Medication adherence
With the personalized approach, coaches also help patients set goals that are connected with them on a personal level. For example, a lifestyle-related goal may be to regain the energy to play with a grandchild, or to learn how to cook healthier meals. By setting goals that are meaningful to the individual’s life, the results are more effective.
Technology & data-driven guidance
Technology is used to communicate one-on-one with patients, and is also used to collect and measure data to drive care plan guidance. Cecelia Health leverages the Glooko diabetes remote monitoring platform to provide data and insights to both the CDCES and the patient. Real-time, smart, data-driven insights are key for improving patient care at scale.
- Provider dashboards
- Population management
- Clinical, fitness and wellness apps
- CGMs and meters
- Connected devices
- Blood pressure and ECG
Proven Outcomes Impacting HEDIS and Star Measures
Results and Clinical Outcomes
Financial Outcomes Lowering per-patient Costs
Complementing Value-Based Programs
Value-based care is a paradigm shift in the healthcare reimbursement structure. No matter the priority of value-based programs, the right approach is needed to support these programs and make them successful for patients, providers, and payers alike. The following should be considered when working to improve quality measures for diabetes care in a value-based model.
| PROGRAM PRIORITY | IMPACT & APPROACH |
|---|---|
| Provide High Value Care | Help identify needs and treatment plan throughout transition of care |
| Improve Health Outcomes | Focus on A1C reduction, medication adherence, closing care gaps and improving self-management confidence |
| Impact Efficiency & Coordination of Care | Extension of care team to reinforce guidelines, care protocols and processes between episodic encounters |
| Enhance Member Experience | Forming personal connections through empathetic, trust building – treating the “person inside the patient” |
| Value Based Purchasing | Support the implementation of the doctor’s care plan and help the providers meet targeted performance goals |
