When we talk about integrated care, it’s easy to dismiss it as another healthcare buzzword. But at Cecelia Health, integrated care is a daily practice—a coordinated effort across licensed clinicians, dietitians, specialty providers, and care navigators who work in sync to support the full health picture of every patient.
Let’s explore what integrated care looks like in action—and why this approach is unique in improving outcomes and reducing costs for members with complex chronic conditions.
Meet Helen
Helen is 52. She lives in a semi-rural area and works full-time. She’s managing:
- Type 2 diabetes
- Obesity (BMI >35)
- Hypertension
- High cholesterol
- She’s also just been prescribed a GLP-1 medication by her PCP.
Helen’s providers are overwhelmed, and don’t have the capacity or resources to support her anytime she has a question. Things like managing medication adjustments, side effects, and screening for nutritional needs, depression, and anxiety in between visits.
For Helen, she doesn’t have time for additional appointments during the workday. With limited access to specialty providers she doesn’t have many options, adding to her stress.
That’s where our team steps in.
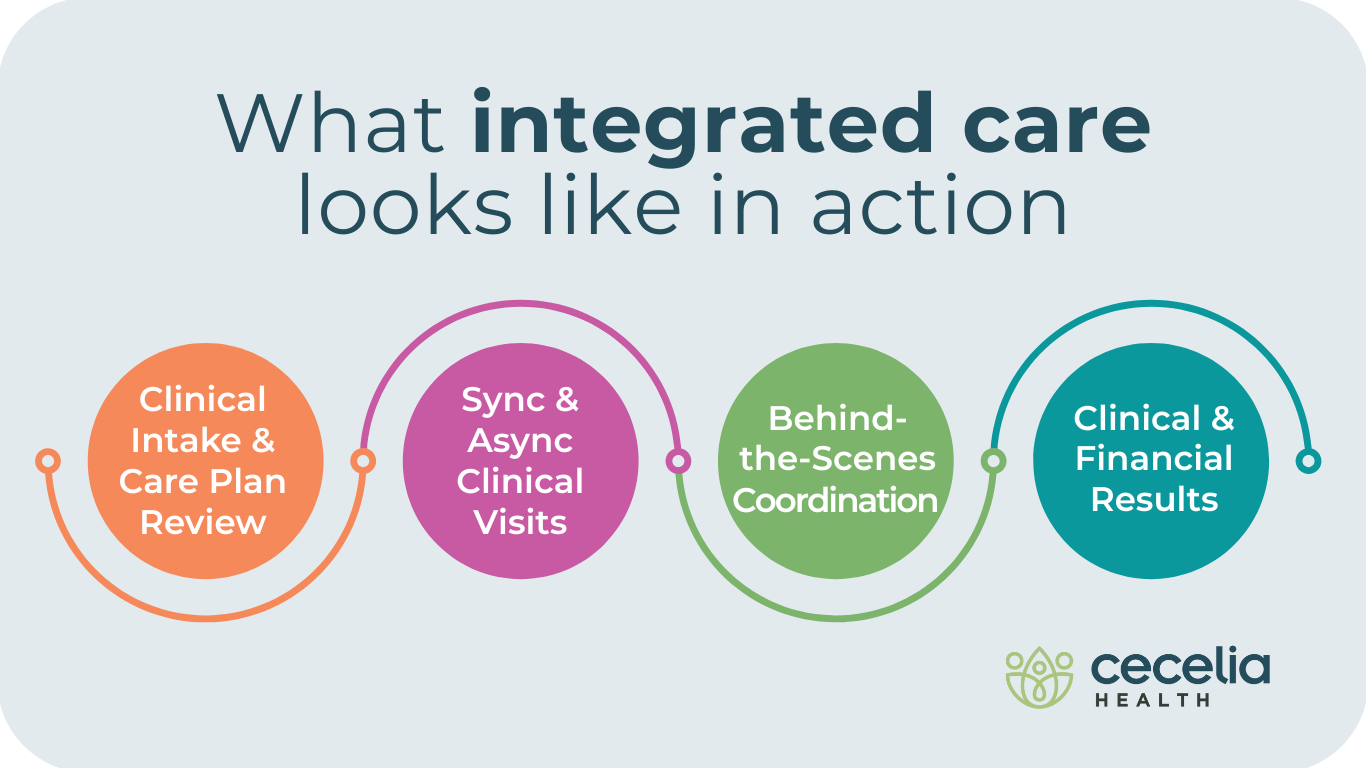
Clinical Intake & Care Plan Review
A Cecelia Health nurse starts with a review of Helen’s chart and conducts a comprehensive initial assessment of her conditions during her onboarding session. This includes screening for depression, anxiety, and social determinants of health, as well as alcohol intake, smoking, sleep patterns, and stress levels assessments.
Based on the initial assessment, the nurse assembles the appropriate care team for Helen—including a Certified Diabetes Care and Education Specialist (CDCES) who is also a registered dietitian (RDN), and a cardiovascular nurse. The team is on the same page to make sure Helen doesn’t trend in the wrong direction:
- Rising blood pressure
- Side effect potential from GLP-1 initiation
- A pattern of medication nonadherence
Synchronous and Asynchronous Clinical Visits
Helen joins a 1:1 virtual visit with her Cecelia Health CDCES to review her GLP-1 titration schedule. They discuss nausea management strategies and her reluctance to exercise due to fatigue. They review Helen’s diabetes management needs and uncover that she is struggling to eat foods that help her regulate blood glucose levels. Helen is asked to connect her CGM and take regular blood pressure measurements so the clinician can monitor her results.
After her visit, Helen’s blood glucose and blood pressure data are available. The clinician sees her blood glucose is improving, but her blood pressure is inconsistent, flagging a possible medication adjustment. The clinician reaches out via chat to discuss with Helen and recommends a medication adjustment. The clinician sends a visit summary to her PCP with the recommendation.
Whether synchronous or asynchronous, every conversation is logged, her care plan is updated, and when necessary, a secure summary is sent to Helen’s PCP to ensure they’re aligned on interventions.
Behind-the-Scenes Coordination
Behind the scenes, Helen’s clinician diligently assesses and coordinates the care she needs. The care is sequenced based on clinical need and her ability and motivation to act. Coordination may look like:
- A Cecelia Health physician checks in to ensure there are no drug interactions with Helen’s antihypertensive medications.
- An alert from Helen’s connected blood pressure monitor flags an elevated morning reading. A Cecelia Health clinician reaches out to check in and sends Helen some clinical education on reducing her sodium intake in her diet.
- Helen’s care team meets weekly to discuss any changes that may be needed to her care plan and discuss guidance for her next virtual visit.
This kind of virtual care isn’t theoretical—it’s what Cecelia Health does every day. We are a single and powerful line of care—not one more disconnected tool in a fragmented system
What Makes it Work
- We are a licensed virtual specialty medical practice with a national network of licensed professionals across multiple specialties.
- We use real-time data to drive decisions and escalate concerns before they become costly.
- We coordinate care with primary and specialty providers—not compete with them.
- We practice whole person care – with clinical, behavioral and nutritional support and sustainable lifestyle interventions.
The Result?
✔️ Higher engagement that leads to patient empowerment
✔️ Fewer urgent care or ER visits
✔️ Lower GLP-1 and comorbid medication costs
✔️ Better satisfaction—for both patients and providers
Let’s Build This Together
If your plan is looking to drive better outcomes and control costs for high-risk members like Helen, let’s connect.