Watch the highlights and key takeaways of our live webinar here:
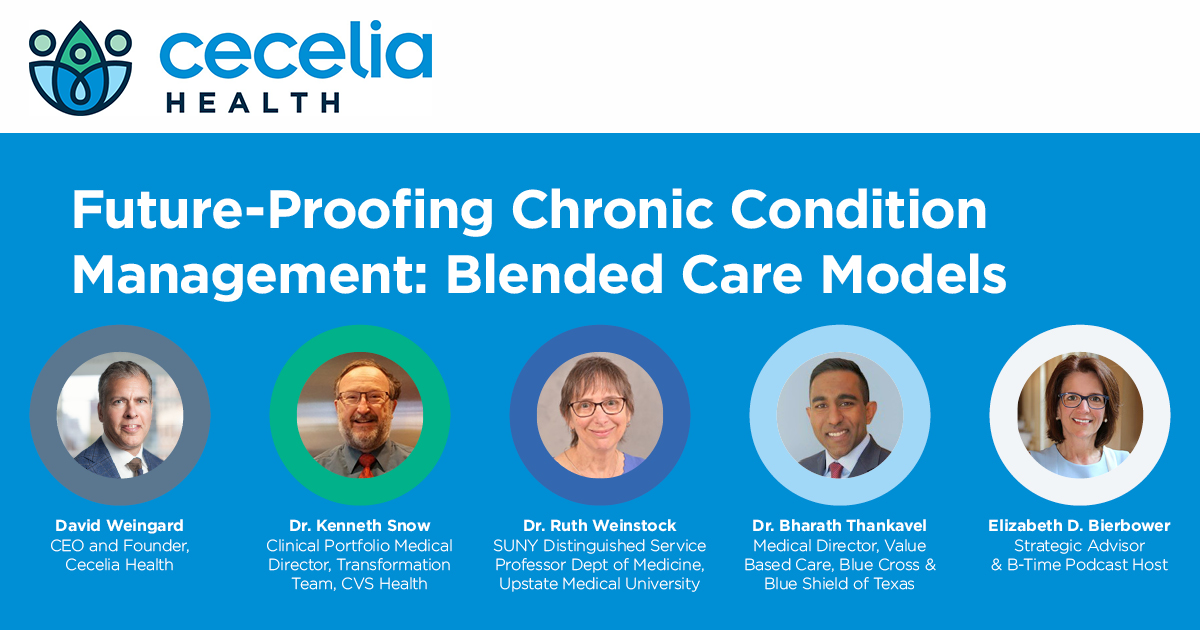
Featured Speakers:
- Dr. Ruth Weinstock, Medical Director, The Joslin Diabetes Center SUNY Upstate Medical
- Dr. Kenneth Snow, Clinical Portfolio Director, Transformation Team, CVS Health
- Dr. Bharath Thankavel, Medical Director, Value Based Care, BCBS TX
- David Weingard, Founder & CEO, Cecelia Health
Panel Discussion Moderated by:
- Elizabeth Bierbower, Strategic Advisor & B-Time Podcast Host
Overview:
On December 8th, a panel featuring healthcare industry thought leaders gathered virtually to discuss the implications of the COVID-19 pandemic and its causative impact on the acceleration of digital health and blended care models for chronic care delivery in the United States. The panelists, senior leaders from the provider, payer, and healthcare innovator communities, drew on their extensive experience in chronic condition management to offer rich insights on the promise of blended care delivery and what it will take for us to establish this model as the standard in care.
Key Takeaways:
The Current State of Chronic Condition Management in America
1.) Most people with diabetes and other chronic conditions are under the care of their primary care provider. The majority don’t have access to the frequent specialty care that they need. If they do, they generally are only able to engage them on a limited basis thus not receiving the frequent interactions they need. A team-based approach combining coaching and care from a primary care provider, coach (CDCES), and specialist (endocrinologist) is optimal.
2.) Far too often in the United States, the zip code you live in is the biggest predictor of health outcomes if you have a chronic illness. If you happen to live in a well-serviced area where you have ready access to qualified providers, your outcomes are likely to be much better than if you happen to be in an underserved area where it’s more of a challenge to receive the quality of care that you need. Virtual care shows promise in equalizing this zip code disparity in chronic condition care.
3.) At present, a significant misalignment of incentives exists in our nation’s healthcare system; often actors are not operating with the most appropriate priorities. The present incentive structure that currently exists often pits important stakeholders against each other which is unquestionably suboptimal for patients, particularly those with chronic illness.
4.) The statistics suggest that we currently find ourselves in a crisis in this country with 1 in 3 Americans predicted to have diabetes by the year 2050. Given that diabetes is a 24 x 7 condition, personalization from both a care and engagement perspective is essential to meet the needs of individuals. Unfortunately, far too few receive the personalized care that they need to optimally manage their diabetes or other chronic conditions.
Why Are Diabetes and Other Chronic Conditions So Hard to Manage?
1.) Chronic diseases are extremely complex. A disease like diabetes interacts with every single choice that you make daily; therefore, individuals often need to be thinking about how to manage their disease every minute of every day. People need a clinical expert to teach them how to use all the tools available to them, analyze their physiological data, and to help them stay accountable.
2.) According to Dr. Ruth Weinstock, there are several factors that prevent providers from optimizing care delivery to ensure positive outcomes for their patients.
-
- Demand from patients is off the charts as diabetes incidence in America continues to grow leading to overburdened specialty clinics.
- Limited care capacity prevents providers from conducting necessary follow up visits and the ability to efficiently and effectively conduct these visits in a timely manner.
- Maintaining effectiveness of patient visits has become challenging given that so many patients struggle with their connected medical devices and physicians have to focus on troubleshooting technology as opposed to optimizing care plans.
3.) Chronic diseases like diabetes require frequent interactions; present policies and means of care delivery don’t facilitate ease of engagement with expert clinicians. It’s simply not convenient for people to access care in the “traditional” sense that would require individuals to take days off from work or drive to a physician’s office. The most promising programs are those that provide for more direct interventions while also integrating into individuals lives either virtually or in the pharmacy.
Making Blended Care a Permanent Fixture in Chronic Condition Management
1.) The shutdown of in-person care visits at places like SUNY Upstate Medical required an overnight transformation to a telehealth-enabled model. SUNY Upstate was able to partner with Cecelia Health to improve care capacity by adding a team of Certified Diabetes Care & Education Specialists (CDCES). Cecelia Health’s ability to provide device coaching, lifestyle education, and telemedicine support proved that a blended care model was highly effective.
2.) Diabetes and many other chronic conditions are unique in that many of the necessary interactions can be done remotely. You don’t need a specialist to start someone on many devices and primary care physicians don’t have the time to manage all intensive requirements to help someone with a disease like diabetes; they can be done by a CDCES. More partnerships between primary care providers and CDCESs should become the new normal.
3.) According to Dr. Snow, virtual care isn’t going anywhere as it has proven its efficacy and convenience during COVID-19. Patients are not going to want to give this up quietly. As both an executive at payer organization CVS Health and a provider, he’s believer in the ability of such practices to be able to localize care by bringing it directly into the homes of patients through both synchronous and asynchronous virtual visits. For many appointments, there is no reason for patients and providers to have to be in the same place at the same time.
4.) It’s essential that policy makers and payers make it as easy as possible for virtual care to continue so that it’s not overly challenging. Additionally, according to Dr. Thankavel of Blue Cross and Blue Shield of Texas, payers should carefully evaluate what is most efficient for them from a care management standpoint and a funding standpoint. It may be more effective from a patient standpoint to outsource care management or to provide funds to providers like SUNY Upstate Medical to be able to establish partnerships with digital health companies like Cecelia Health.
To advance change for the best interest of patients living with chronic illness in the United States, more rich dialogue between payers, providers, and solution providers is critical.
Watch the full webinar here:
About the Author

Daniel Johnson has been with Cecelia Health since January 2020. Prior to joining Cecelia Health, Daniel held marketing, operations, and policy roles at McKesson Corporation supporting leading pharmaceutical and pharmacy customers achieve their strategic marketing, distribution, and sales goals. Prior to joining McKesson, Daniel worked in Marketing at Pfizer and held various roles with Teach For America as a Corps Member and Recruitment Strategy Manager. He holds BA from Boston College, and M.Ed. from the University of St. Thomas, and an MBA from the University of North Carolina, Kenan-Flagler Business School. Daniel Johnson has been with Cecelia Health since January 2020. Prior to joining Cecelia Health Daniel held marketing, operations, and policy roles at McKesson Corporation supporting leading pharmaceutical and pharmacy customers achieve their strategic marketing, distribution, and sales goals. Prior to joining McKesson, Daniel worked in Marketing at Pfizer and held various roles with Teach For America as a Corps Member and Recruitment Strategy Manager. He holds BA from Boston College, and M.Ed. from the University of St. Thomas, and an MBA from the University of North Carolina, Kenan-Flagler Business School.
Get in contact with Daniel:
Email: danieljohnson@ceceliahealth.com
LinkedIn: Daniel Johnson