By Dr. Arnold Saperstein, CMO
In the dynamic landscape of healthcare, employers and health plans are shifting toward integrated chronic care management to improve clinical outcomes, enhance the patient experience, and reduce medical care costs. These solutions target a range of conditions—such as diabetes, hypertension, and obesity, while addressing behavioral health needs—resulting in more comprehensive and effective care. In contrast, point source solutions, while effective for single diagnoses, fall short when individuals are simultaneously managing multiple chronic conditions.
The Challenge of Comorbidities
Frequently, individuals with one chronic condition contend with comorbidities—conditions interlinked in complex ways. For instance, poorly controlled hypertension and/or diabetes often lead to chronic kidney disease (CKD), which, in turn, is linked to the progression of cardiovascular diseases. Additionally, individuals diagnosed with diabetes, especially Type 2, are commonly overweight, increasing the risk of poor diabetes control and heightened cardiovascular risk.
Currently, it’s estimated that more than two in five adults in the U.S. suffer from more than one chronic condition.
- Nearly 3 in 4 adults with diabetes have hypertension1; 1 in 3 has CKD.2
- Studies suggest that 20% to 30% of adults with hypertension have diabetes.
- Of adults with CKD, 36% to 84% also have hypertension, depending on stage,3 and 44% have obesity.4
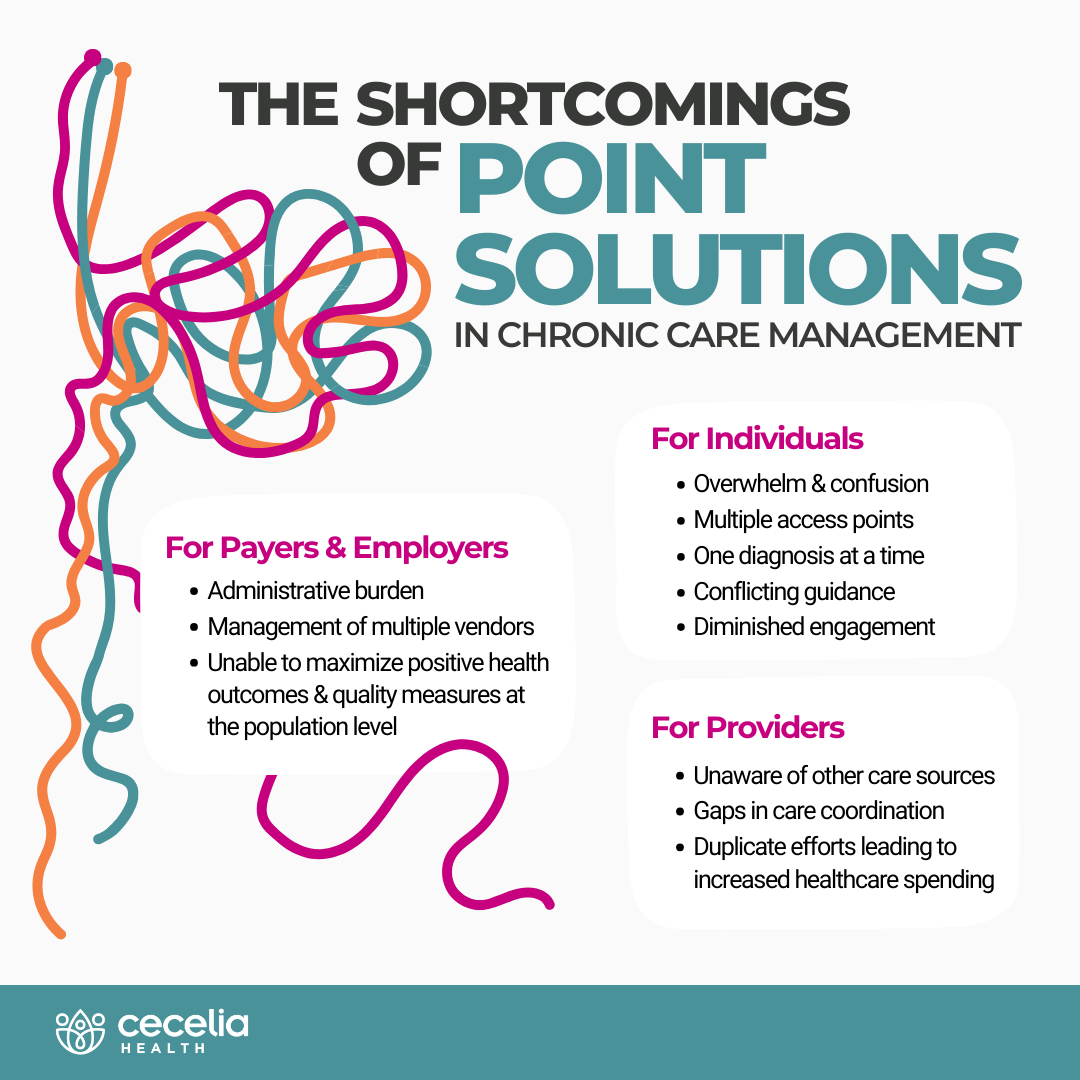
The Shortcomings of Point Solutions
With the potential of multiple chronic diseases, and the complex interconnected risks associated, managing individuals and improving outcomes becomes challenging through a variety of point solutions:
- Individuals receiving care can easily become overwhelmed and confused, leading to diminished engagement. Juggling separate programs, each addressing a singular diagnosis while requiring multiple touchpoints, becomes a daunting task hindering the potential for positive outcomes. Also, there are varied levels of risks for individuals if they receive conflicting guidance between disparate, disconnected solutions related to their nutrition or lifestyle behaviors.
- Providers, whether primary care physicians (PCP) or specialists, on an individual’s care team may be unaware of the guidance their patient is receiving from other sources. This creates gaps in care coordination or, perhaps more costly, duplicates efforts.
- Payers and employers bear the administrative burden of vetting and implementing solutions across multiple vendors with distinct workflows, systems, and service-level agreements. Much of this inefficiency could be overlooked if these solutions were producing results; however, point solutions have yet to prove their sustainability for maximizing population-level outcomes while improving overall quality (i.e., HEDIS and STAR measures).
The Power of Integrated Chronic Care
Comprehensive and well-coordinated healthcare has a much greater potential to achieve positive clinical outcomes and reduce morbidity, especially for individuals managing multiple chronic conditions.
- A path to true personalization: A comprehensive view of an individual’s health allows care teams to understand how chronic conditions—such as diabetes, CKD, and hypertension—intersect and influence one another. This holistic perspective enables more informed and personalized care plans tailored to the specific needs of the individual.
- Enhanced patient engagement: Integrated chronic care empowers individuals to actively participate in their healthcare journey. When they understand the relationships between their chronic conditions and the impact of lifestyle choices, individuals are more likely to engage in self-management practices. This empowerment can lead to improved adherence to care plans, healthier behaviors, and a better overall quality of life.
- Prevention and early intervention: Proactive measures and early intervention strategies are facilitated by integrated chronic care teams. By recognizing the interconnected nature of chronic conditions, potential complications or exacerbations can be identified before they escalate. This proactive approach aids in preventing complications and managing conditions more effectively, ultimately reducing the risk of hospitalizations and emergency interventions.
- Expanded access to specialized expertise: Collaboration enables existing care teams and care management programs to tap into a broader range of expertise and fill gaps, including those created by capacity or resource limitations. This results in more comprehensive care plans and increases patient access to specialty care and support.
- Efficient & cost-effective care: Integrated chronic care eliminates much of the risk related to fragmented care and redundant healthcare spending (e.g., multiple providers requesting the same lab tests). Additionally, health plans and employers choosing a single vendor benefit from a centralized system, streamlined operations and workflows, reduced administrative costs, and better utilization of resources.
We can redefine specialty care delivery by addressing the whole person across multiple disease states through integrated chronic care to foster greater efficiency and better outcomes. Contact us today to learn more about the transformative impact of an integrated care approach.
Sources
- Naha S, Gardner MJ, Khangura D, et al. Hypertension in Diabetes. [Updated 2021 Aug 7]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279027/.
- Chronic Kidney Disease (CKD). Centers for Disease Control and Prevention. Accessed 1 Feb 2024 from https://www.cdc.gov/diabetes/managing/diabetes-kidney-disease.html.
- Tedla FM, Brar A, Browne R, Brown C. Hypertension in chronic kidney disease: navigating the evidence. Int J Hypertens. 2011;2011:132405. doi: 10.4061/2011/132405. Epub 2011 May 24. PMID: 21747971; PMCID: PMC3124254. Available from: https://pubmed.ncbi.nlm.nih.gov/21747971/.
- Kreiner FF, Schytz PA, Heerspink HJL, von Scholten BJ, Idorn T. Obesity-Related Kidney Disease: Current Understanding and Future Perspectives. Biomedicines. 2023; 11(9):2498. https://doi.org/10.3390/biomedicines11092498.
About the Author

Dr. Saperstein began his managed care career in 1992 and continues to dedicate his expertise to developing programs that ensure the highest quality of care. He joined Cecelia Health in 2019 as Chief Medical Officer, where he built the first national virtual Endocrinology telemedicine practice. Dr. Saperstein has expanded the company’s chronic disease management approach beyond Diabetes to include Cardiovascular risk reduction, Congestive Heart Failure, Obesity, Chronic Kidney Disease, Asthma, and COPD programs.
Dr. Saperstein leads Cecelia Health’s national network of expert clinicians and specialty providers, achieving excellent clinical results for patient populations across the country. Prior, Dr. Saperstein held leadership positions at MetroPlus Health Plan, joining in 1995 as Chief Medical Officer, next serving as President and CEO from 2006 until 2019. Under his leadership, MetroPlus ranked as one of the highest scoring plans for quality of care (measured by the New York State Department of Health Medicaid Incentive Program and by the Medicaid Consumer Guide for New York City) and rose to the forefront of Value Based Purchasing. During his tenure, Dr. Saperstein developed a groundbreaking quality incentive pay for performance program across the entire network of an estimated 32,000 providers and grew the member population 1100% to serve more than 500,000 people.

