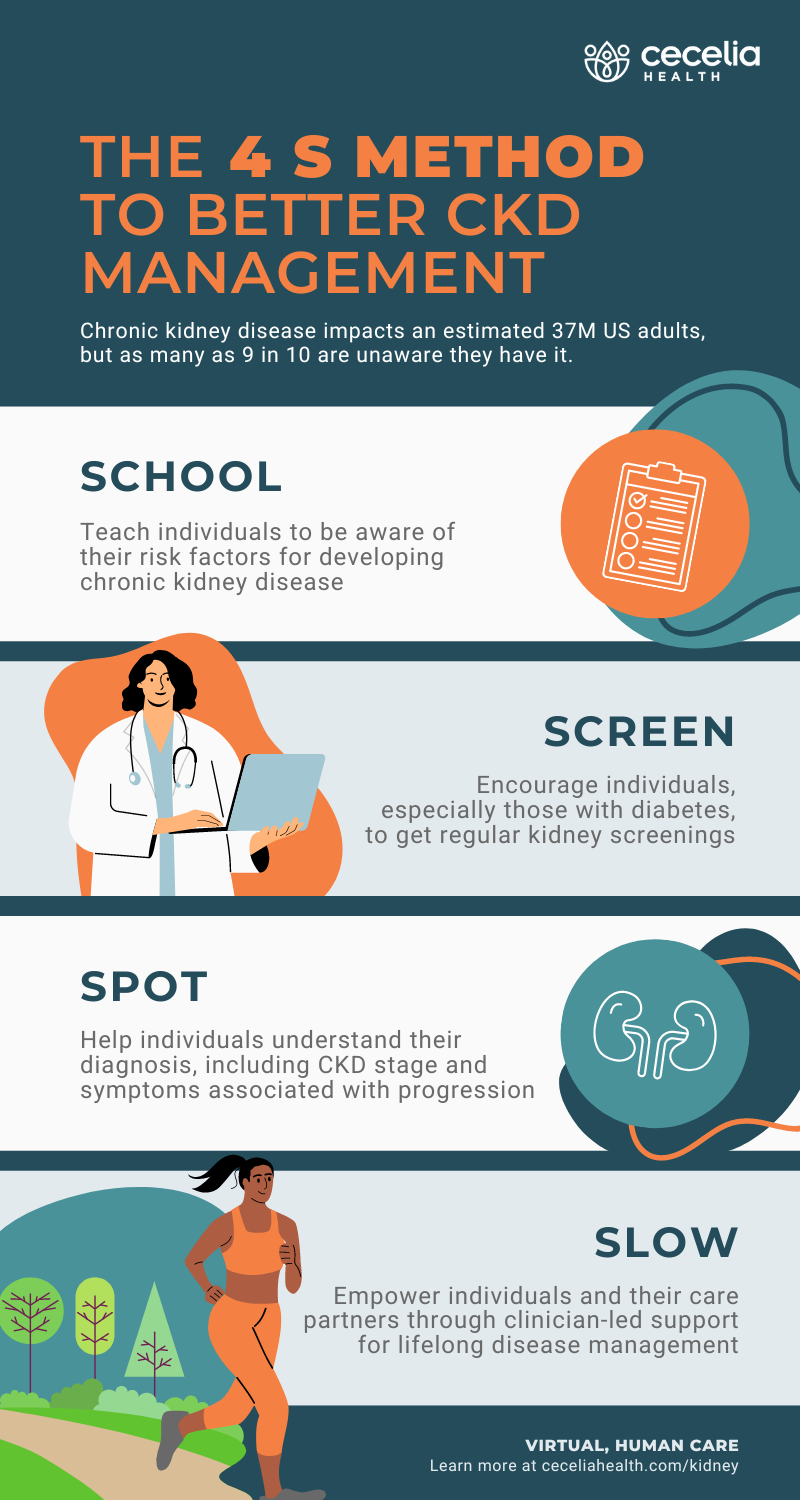
37M adults in the US are estimated to have chronic kidney disease (CKD but as many as 9 in 10 are unaware they have it. (source) How can you build effective chronic care management programs to address CKD if the majority of your impacted population isn’t aware of their status?
Below, we outline the “4 S Method” to promote better CKD management across your population.
School
First, it’s important for your members to have an awareness of (or be “schooled” on) what can lead to an increased likelihood of CKD diagnosis. Many factors are at play including obesity, family history, and age, but there are two primary causes of CKD—diabetes and hypertension (or high blood pressure).
- 1 in 3 adults with diabetes (type 1 and type 2) have a CKD diagnosis CKD (source)
- Nearly 30% of adults with diagnosed hypertension also have a CKD diagnosis (source)
Once individuals understand their risk, the next step is to check kidney function.
Screen
In many cases, kidney disease is asymptomatic until it has progressed to a more advanced stage. Therefore, kidney screenings are essential for early detection and treatment. However, less than 50% of people with diabetes receive an annual kidney screening (source).
Even with a CKD diagnosis, individuals need regular kidney function testing to ensure their condition is being managed effectively and allow for timely adjustments in their treatment plan.
A new HEDIS measure, introduced in 2020, aims to close gaps in care and improve testing for people with diabetes. Not only does this promote proactive healthcare for individuals, but it also helps health plans like yours reduce total cost of care by managing CKD before it progresses to kidney failure.
Spot
A CKD diagnosis includes a classification into one of five stages, with 1 being the mildest and 5 being the most severe (also known as ESRD, end-stage renal disease). In addition, your members with CKD are also at increased risk of developing other health complications, such as cardiovascular disease, anemia, and bone disease. (source, source, source)
Treatment typically involves management of underlying conditions, such as high blood pressure and diabetes, but also medication management, nutrition changes, and lifestyle modifications to manage symptoms and maintain quality of life while slowing disease progression.
Indeed, your members and their care partners have a lot of information to absorb at the point of diagnosis and in the months following. They need to fully understand what CKD is, the role of their kidneys in overall health, and long-term risks related to poor management. Further, they need to know how to manage CKD in conjunction with their underlying conditions. Managing diabetes or hypertension alone requires daily commitment and overcoming challenges—when CKD is introduced, it can become overwhelming. For example, how do you develop a nutrition plan that brings together both diabetes- and CKD-related needs?
Clinical support and education from disease state experts can lessen the burden on healthcare providers and improve the patient experience by providing guidance in between appointments to ensure people are remaining adherent to care plans and have emotional support to navigate the changes necessary for improved health.
Slow
Since CKD is a progressive condition where kidneys gradually lose their ability to filter waste and excess fluid from the body, adherence to treatment plans is critical to avoid kidney failure, dialysis, or transplant. There are several steps a patient can take to slow the progression of CKD and maintain, or even improve, their quality of life:
- Control blood pressure
- Manage blood sugar
- Adopt a healthy diet that is low in sodium, saturated fats, and processed foods; limit intake of high potassium and phosphorus-rich foods
- Exercise regularly and appropriately for individuals with kidney disease
- Smoking cessation
- Take medications as prescribed
Ongoing education and support are essential, but oftentimes individuals and their care partners need more support beyond doctor visits to fully embrace the lifelong changes that are required to slow progression of the disease.
How to implement a CKD management solution that works
Slowing the progression of CKD and preserving kidney function requires a combination of lifestyle changes, medication management, and close monitoring by a healthcare provider. This can be overwhelming and discouraging for many individuals who lack access to support and resources for daily management. Lifestyle changes alone require a lifelong commitment that starts with gradual steps to meet health goals.
With support from credentialed clinicians and specialists, like those who support Cecelia Health’s virtual specialty care programs, your members will have a disease state expert who will help them navigate life with CKD. Learn more about our approach to better kidney health.